My Personal Story with Rabies: From a Jaguarundi to a Vaccine.
- Cristian Porras Ramírez

- Sep 6, 2025
- 19 min read

I had never been vaccinated against rabies because I thought I would never need it. However, I recently had an incident with a jaguarundi in Guatemala that made me reconsider my perception of vaccines and the preventive measures we often overlook in such situations.
Fortunately, the neonate did not seem to show signs of rabies, but this experience reminded me of a harsh reality: rabies is one of the deadliest viruses in human history, with a case fatality rate of nearly 100% once clinical symptoms appear. In other words, if preventive treatment is not administered in time, survival is almost impossible.
In Costa Rica, there have been no locally acquired human rabies cases reported for decades. In fact, the last documented case of canine rabies dates back to 1987, and since then, no human cases acquired locally have been recorded.
In the Neotropics, human rabies cases are rare but not nonexistent. Between 2000 and 2022, there were 339 reported cases of human rabies transmitted by hematophagous bats, with the Amazon region being one of the most active hotspots, where cases tend to occur in cyclical outbreaks.
For those of us working with wildlife in the Neotropics —or anywhere in the world— getting vaccinated against rabies is something we often don’t think about… but definitely should.

Historical Origins of Rabies
Rabies is one of the oldest recognized infectious diseases. Historical records of a “madness” transmitted through animal bites date back almost 4,000 years. Texts from ancient Mesopotamia (circa 2300–2200 B.C.) describe rabid dogs and establish fines for owners who failed to prevent bites.
The very word “rabies” comes from the Latin rabere, meaning “to rage”, referring to the furious aggression observed in rabid animals.
In the 4th century B.C., Aristotle noted that “if a rabid dog bites, all animals bitten become rabid”, thereby recognizing the transmissibility of the disease.
Similar accounts appear in early medical texts worldwide. For example, a 1st-century A.D. Indian manuscript (Susruta Samhita) describes the symptoms of rabies —often referred to as hydrophobia, or fear of water.
During the Middle Ages, rabies was universally feared as an “ancestral curse”, invariably fatal once symptoms appeared.
A turning point came in 1885, when French scientist Louis Pasteur developed the first effective rabies vaccine. Pasteur famously saved a 9-year-old boy, Joseph Meister, by administering a series of inoculations after the child was bitten by a rabid dog —the first known successful post-exposure treatment against rabies.
This breakthrough ushered in the era of prevention, transforming rabies from a deadly curse into a disease that could be controlled through science.

Taxonomy and Biology of the Virus
Rabies is caused by a virus of the genus Lyssavirus, within the Rhabdoviridae family. The rabies virus (Rabies lyssavirus) has a bullet-shaped structure and is enveloped, measuring approximately 75 nm in diameter and 180 nm in length.
It carries a negative-sense, single-stranded RNA genome of about 12,000 bases. Like its relatives, it encodes five major proteins, including a glycoprotein that allows it to infect nerve cells.
There are numerous species of Lyssavirus —over 17 identified so far— found in bats and other mammals worldwide. However, the rabies virus proper (sometimes called genotype 1 lyssavirus) is the most widespread and significant, responsible for the vast majority of animal and human cases.
All mammals are susceptible to rabies virus infection, which can invade the central nervous system. After a typical exposure (such as a bite), the virus travels along peripheral nerves toward the brain, a journey that can take weeks or months. Once it reaches the brain and begins to replicate, it causes acute encephalitis —inflammation of the brain— which is ultimately lethal.
Importantly, rabies is a zoonotic disease, meaning it can be transmitted from animals to humans. The virus circulates in both wildlife and domestic animals, so its control requires an integrated approach involving veterinary medicine and human healthcare.
Transmission and Symptoms in Animals and Humans
Rabies is primarily spread through the saliva of infected animals. A bite from a rabid animal is by far the most common route of transmission to both humans and other animals. Scratches or any exposure of the mucous membranes (eyes, mouth) or broken skin to saliva or nervous tissue can also transmit the virus. In the context of human cases, domestic dogs are the source of infection in about 99% of cases worldwide, which is why dog bites are a central focus of prevention.
Other mammals can also transmit rabies: bats, cats, foxes, raccoons, skunks, mongooses, and other carnivores can harbor the virus. It is not transmitted through intact skin or casual contact (you do not get it by petting a rabid animal, nor from its blood, urine, etc.; the risk lies in contact between infected saliva/nerve tissue and your tissues).
While bites are the typical route, a few unusual cases have occurred. For example, inhalation of the virus in caves with abundant bats, consumption of raw products from infected animals, or organ transplants from donors with undiagnosed rabies have led to infections in extremely rare instances. Direct person-to-person transmission (via bites or saliva) is theoretically possible, but it has never been confirmed in documented cases. In short, any mammal bite that punctures the skin should be treated as a possible rabies exposure, especially if the animal is behaving abnormally or if rabies occurs in the region.
Symptoms
Rabies has an incubation period in humans that typically ranges from 2 to 3 months, though it can be as short as one week or as long as one year. Early on, the person or animal may show general, nonspecific symptoms: fatigue, fever, headache, and sometimes pain or tingling at the bite site. These early signs make initial clinical diagnosis in humans difficult. As the virus progresses toward the central nervous system, severe neurological symptoms appear. In humans, rabies presents in two forms:
Furious rabies
The classic and most common form (approximately 80% of human cases). It is characterized by hyperactivity, extreme agitation, confusion, hallucinations, and aggressive behavior. During this phase, spasms of the throat muscles trigger hydrophobia—an infamous symptom in which the patient panics or chokes at the sight of water and cannot drink. Aerophobia (fear of air currents) can also occur due to heightened nerve sensitivity. Other signs include excessive salivation—the classic “foaming at the mouth”—and difficulty swallowing. Seizures or fasciculations may occur, and coordination is lost. Animals with furious rabies often show extreme aggression or, paradoxically, unusual tameness; wild animals may approach people without fear. This phase is brief and severe: after a few days, the patient goes into cardiorespiratory arrest and dies.
Paralytic rabies
A less dramatic form (around 20% of human cases), also called “dumb rabies.” Instead of hyperactivity, weakness and paralysis predominate, beginning at the bite site and gradually spreading through the body. The victim becomes lethargic, may show confusion, and eventually falls into a coma. Because it lacks the violent signs, paralytic rabies can be harder to recognize and is sometimes misdiagnosed (for example, as Guillain–Barré syndrome or other neurological disorders), contributing to underreporting. The outcome is the same: after a somewhat longer course than furious rabies, paralysis progresses to coma and death from respiratory failure.
Signs in animals
In animals, the signs mirror those seen in humans. Early on, an infected animal may simply appear ill or altered. Neurological symptoms soon develop: wild animals may lose their natural fear of humans, and normally friendly pets may become shy or irritable. As the disease advances, animals typically exhibit either the furious form (growling, indiscriminate biting, erratic wandering, snapping at the air) or the paralytic form (weakness, incoordination, up to complete paralysis). A commonly depicted sign is excessive salivation and foaming at the mouth, caused by pharyngeal spasms that prevent swallowing and allow saliva to accumulate as foam. Other signs include howling or abnormal vocalizations, disorientation, and seizures. Cattle and horses may show unusual bellowing or unprovoked aggression. Ultimately, a rabid animal falls into a coma and dies—usually within a week of onset. It is important to remember that not all rabid animals foam at the mouth or act aggressively: the absence of those signs does not guarantee that an animal is not infectious. Any mammal behaving unusually (e.g., a nocturnal species active during the day or a wild animal that approaches people) should raise suspicion.
Nearly 100% Fatality in Symptomatic Rabies
Rabies is the most lethal infectious disease known. Once the virus reaches the victim’s central nervous system and clinical symptoms begin, the disease is virtually 100% fatal. In fact, it has the highest case fatality rate of any conventional disease: essentially, almost 100% of unvaccinated victims die after the onset of symptoms. Only a handful of people in history have survived rabies once symptoms had started, and those cases involved experimental and intensive medical care (for example, the “Milwaukee protocol”) and often resulted in long-term neurological sequelae. In practice, there is no cure once the disease manifests; treatment at this stage is mainly supportive (palliative care).
This reality explains why rabies is so feared and why prevention is absolutely critical. The virus causes irreversible damage to the brain and spinal cord, leading to delirium, seizures, and death despite any intervention.
However —and this is crucial— rabies deaths are entirely preventable if the exposed person receives proper medical attention before symptoms appear. The following section explains how timely vaccination can prevent this tragedy.

Global and Neotropical Rabies Statistics
Rabies represents a public health threat on all inhabited continents, being present in more than 150 countries, and causes tens of thousands of human deaths every year. A key figure cited by the World Health Organization (WHO) is approximately 59,000 human deaths annually due to rabies, although this figure is likely underestimated because of poor reporting in some regions. The burden is overwhelmingly concentrated in developing regions of Asia and Africa, which account for about 95% of all human deaths. Within these communities, children are especially vulnerable: approximately 40% of rabies victims are under 15 years old, as they are more likely to approach animals and less likely to report minor bites.
The economic cost is also enormous, estimated at around USD 8.6 billion per year globally, considering healthcare costs, lost income, and dog vaccination campaigns —not including the immeasurable emotional trauma. Despite these alarming numbers, rabies remains a neglected tropical disease in many areas, meaning it has historically received less attention and funding relative to its impact.
In Latin America (Neotropical region), the Americas have achieved major progress in rabies control, particularly the canine form (transmitted by dogs). Thanks to vaccination campaigns and public health initiatives implemented since the 1980s, Latin America has seen a 95% reduction in both human and canine rabies cases over recent decades. In 1983, an international program supported by the Pan American Health Organization (PAHO) was launched to eliminate human rabies transmitted by dogs, achieving remarkable results. By 2017, the entire Latin American and Caribbean region reported only 19 human cases in that year, concentrated in just four countries: Bolivia, Guatemala, Haiti, and the Dominican Republic.
The vast majority of Central and South American countries reported zero human cases and zero canine cases that year, demonstrating the effectiveness of mass vaccination and stray animal control measures in nearly eliminating canine rabies. By 2018, canine rabies remained endemic only in those four countries, while most other nations in the region had either completely eliminated it or reduced it to sporadic, isolated incidents. Some countries —such as Brazil, Cuba, and Peru— still occasionally report a rabid dog, but these represent only a small fraction of total infections.
This regional success is considered a global model for rabies control, proving that mass vaccination of dogs —covering at least 70–80% of the canine population in high-risk areas— can effectively break the transmission cycle to humans, since dogs have historically been the primary vector. As canine rabies decreases, most remaining human cases in the Americas are now linked to wildlife exposure, especially bats. Overall, the region is moving steadily toward the goal of zero human deaths from dog-transmitted rabies. Health authorities continue to vaccinate millions of dogs annually and ensure timely access to post-exposure treatment for bite victims, in order to maintain these achievements and achieve the total elimination of canine rabies.
For reference, many other regions of the world have also eradicated canine rabies: the United States and Canada have been free of canine rabies for decades; Western Europe eliminated canine rabies by the late 20th century; and countries such as Japan, South Korea, and several island nations are also considered rabies-free. However, these regions remain highly vigilant, as rabies can re-enter through imported animals or wildlife reservoirs, making continuous surveillance and pet vaccination essential.
Importance of Vaccination and Timely Treatment (Pre- and Post-Exposure)
Rabies is preventable through vaccination —both in animals and humans. Modern cell-culture vaccines are safe and effective, and their strategic use is the cornerstone of rabies control. In humans, there are two main contexts.
Pre-exposure prophylaxis (PrEP) is a preventive vaccination administered before any potential exposure, recommended for people at high risk of encountering rabies. PrEP generally consists of a series of two or three doses that prepare the immune system against the virus. It is recommended for laboratory workers handling rabies virus, veterinarians and animal handlers, wildlife researchers, park rangers, and other professionals who are regularly exposed. It is also advised for travelers spending extended time in rural endemic areas or for people living in remote regions with limited access to post-bite treatment.
PrEP does not guarantee that rabies will not be contracted if a bite occurs, but it significantly improves the body’s ability to neutralize the virus quickly. If a person who has received PrEP is bitten, they still require post-exposure treatment, but the protocol becomes simpler, involving fewer vaccine doses and no need for rabies immunoglobulin (RIG). Essentially, PrEP provides a critical time advantage and an extra layer of protection, which can be vital in areas far from medical care.
Post-exposure prophylaxis (PEP) is the emergency treatment administered after a bite or other suspected exposure. When applied promptly —ideally within hours or a few days after exposure and before symptoms begin— PEP is nearly 100% effective in preventing the virus from establishing itself. PEP includes: immediate and thorough wound cleansing (washing the bite site with soap and water, often followed by iodine or alcohol solution, for at least 15 minutes to remove and inactivate as much virus as possible), a series of rabies vaccinations (a regimen lasting a couple of weeks, administered intramuscularly or intradermally using WHO-prequalified vaccines), and in cases of severe exposure —such as multiple bites, bites on the head or neck, or in immunocompromised individuals— the administration of rabies immunoglobulin (RIG), injected both around the wound and intramuscularly, to provide immediate passive immunity while the body generates its own immune response.
Together, these measures stop the virus before it reaches the brain. It is crucial to stress that rabies can be prevented if PEP is administered in time. Therefore, anyone bitten or scratched by an animal in a rabies-endemic area should seek immediate medical attention for evaluation and treatment. The World Health Organization (WHO) recommends never missing an opportunity to administer PEP; even if months have passed since a high-risk bite, treatment may still be considered. Thanks to PEP, tens of thousands of lives are saved each year.
However, significant challenges remain: in some developing regions, access to vaccines and RIG —both costly— is limited, and many patients are unaware of the need for immediate treatment. Public education about what to do after an animal bite —washing the wound and seeking prompt medical care— is essential. In recent years, the WHO has promoted more cost-effective PEP strategies, such as administering the vaccine intradermally rather than intramuscularly, which reduces the dose required per shot while maintaining equal efficacy. This innovation helps expand access to treatment in resource-limited regions.
In the veterinary field, animal vaccination —especially in dogs— is crucial. Mass dog vaccination creates a “herd immunity shield” that drastically reduces transmission to humans. In many countries, dogs are legally required to be vaccinated every year or every two years. Vaccinating wildlife is more complex, but in some cases oral vaccine baits are distributed to control rabies in wild carnivores —for example, campaigns that have eliminated rabies in fox populations across much of Western Europe.
Animal vaccination, combined with PEP in humans, forms a two-pronged strategy: stopping the virus at its animal source while providing a safety net for human exposures.
Rabies in Costa Rica and Regions That Eliminated Canine Rabies
Costa Rica provides an exemplary case of rabies control. This Central American country eliminated rabies transmitted by dogs decades ago through rigorous vaccination campaigns and public health measures. The last human case caused by a dog bite in Costa Rica was reported in the late 1970s. Since then, rabies in domestic animals has been effectively controlled: for more than 40 years, canine rabies has not been a public health problem in the country. The Ministries of Health and Agriculture (with support from the Pan American Health Organization, PAHO) implemented routine dog vaccination and continuous surveillance starting in the 1970s, achieving one of the earliest national eliminations of canine rabies in the Americas. As a result, an entire generation has grown up without fearing rabid dogs on the streets.
However, the story did not end in the 1970s. As in many countries where canine rabies has been controlled, the remaining concern shifted to wildlife reservoirs. The main culprit in Costa Rica (and much of Latin America) is the common vampire bat (Desmodus rotundus). These bats, which feed on the blood of livestock and occasionally on humans, can carry rabies and transmit it to other animals. Costa Rica continues to experience occasional outbreaks in cattle and other animals due to vampire bat bites. Between 1985 and 2014, for example, over 70 bovine rabies outbreaks were documented in the country, resulting in 723 cattle deaths —a significant burden for ranchers in certain regions. All these outbreaks were attributed to vampire bats as the source of infection. The response has included vaccinating livestock in high-risk areas and even targeted control of bat populations around affected zones.
There have also been rare spillover events into other wild species and unvaccinated pets. For example, a rabid jaguarundi (a wild cat) was confirmed in a rural area of the country, illustrating that wild carnivores can also become infected with bat-associated rabies variants. A jaguarundi in Brazil was also found to be rabid in 2024, demonstrating that these events are possible wherever rabies circulates in wildlife.
Crucially, Costa Rica has recorded very few human cases in the past decades, thanks to the elimination of canine rabies and the availability of post-exposure prophylaxis (PEP). After the 1970s, the country went over 30 years without human cases. Then, in 2001, two people in a remote area died from rabies —unusual cases caused by a bat-associated variant, marking the end of a 31-year absence. Investigations found that a vampire bat likely transmitted the virus to a domestic cat, which then bit the victims. More recently, in 2014, another isolated human case occurred —a child who died after being bitten by a bat in a rural area— highlighting the continued need for surveillance.
The good news is that these cases remain extremely rare: the public health system responds quickly to bat exposures, and people at risk (e.g., cavers, bat researchers, and specific rural communities) receive education on rabies prevention and PEP access. Costa Rica’s achievement mirrors that of other countries that have eliminated canine rabies and demonstrates that, with political commitment, coordinated campaigns, and community participation, rabies can be pushed to the margins of wildlife.
In other regions, many parts of the world have also eliminated or drastically reduced canine rabies, historically responsible for most human cases. By 2018, the Americas were close to being canine-rabies-free: only four countries —Bolivia, Guatemala, Haiti, and the Dominican Republic— maintained sustained dog-to-dog transmission, though at much lower levels than in the past.
In Europe, canine rabies was eradicated in Western and Central regions by the early 2000s, thanks to mandatory pet vaccination and oral wildlife vaccination programs designed to prevent foxes from reinfecting domestic dogs. North America (U.S. and Canada) has been free of dog-transmitted rabies for decades —since the 1950s in Canada and 2007 in the U.S.— although strict importation controls and ongoing oral vaccination of wild reservoirs are maintained.
Asia and Africa —where the burden is highest— are carrying out mass canine vaccination campaigns inspired by the Americas’ model, though challenges such as large stray dog populations and resource limitations slow progress. Countries like Mexico and Sri Lanka have already been declared free of dog-transmitted rabies, showing significant advances.
Achieving and maintaining elimination requires constant effort: if vaccination rates decline, there is a risk of re-emergence through uncontrolled dog populations or the introduction of infected animals.
International cooperation and continuous surveillance are essential. The WHO, together with the FAO and WOAH, is driving the global “Zero by 30” initiative, aiming to end human deaths from dog-transmitted rabies by 2030. Countries that have already eliminated canine rabies —such as Costa Rica— offer valuable lessons, including the importance of community involvement and sustained funding.
Wildlife Reservoirs and Conservation Considerations
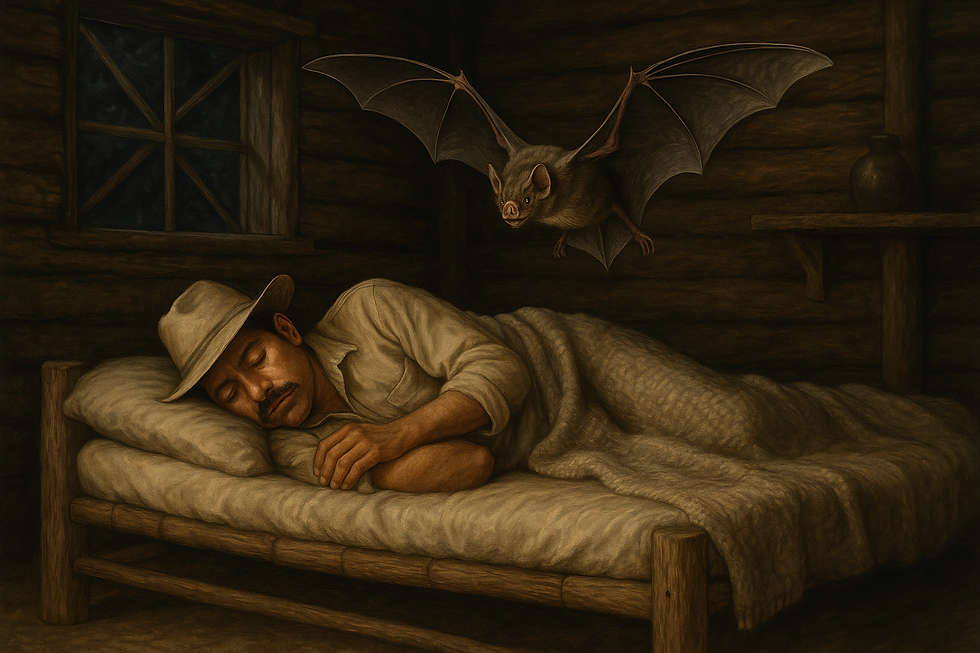
As canine rabies becomes controlled in many areas, wildlife has become the main focus of rabies epidemiology and poses new challenges. Rabies persists in nature thanks to certain wild species that act as reservoirs, allowing the virus to circulate indefinitely within their populations. The most notable example worldwide is bats. Numerous species carry their own variants of rabies-related viruses (lyssaviruses). In the Americas, hematophagous bats —especially the common vampire bat— are currently the primary source of human infections, since dog-to-human transmission has declined.
Bat bites (often occurring while people are asleep or when entering caves) have caused high-profile rabies outbreaks in remote regions of Latin America; for example, in Amazonian communities where vampire bats fed on sleeping people during the night. In North America, where there are no vampire bats, insectivorous bats are also rabies carriers: most recent human rabies cases there have been linked to bat strains. Even in Australia and parts of Europe —traditionally considered free of rabies in terrestrial animals— bat-associated lyssaviruses have emerged, causing rare human cases and prompting public warnings against handling bats.
Beyond bats, terrestrial wildlife maintains rabies cycles in many regions. Classic examples include foxes in Europe and parts of Asia, jackals in Africa, raccoons and skunks in North America, and mongooses in the Caribbean. In the United States, eastern raccoons experienced a large rabies epizootic during the late 20th century, and Texas has faced enzootics among skunks and foxes. In Latin America, aside from bats, rabies cases occur in wild carnivores such as coyotes, foxes, and small wild felines. We previously mentioned that a jaguarundi in Brazil was diagnosed with rabies. Although infrequent, this highlights that any mammalian carnivore can become part of the wildlife transmission cycle if the virus exists in the ecosystem.
These wild cycles sometimes spill over into domestic animals: for example, in Africa, rabid wild carnivores can transmit the virus to unvaccinated dogs or livestock.
From a conservation perspective, rabies presents a double-edged challenge. On one hand, it threatens endangered species: the Ethiopian wolf, one of the rarest canids in the world, has suffered population declines due to rabies introduced by domestic dogs. Conservationists have implemented emergency vaccination campaigns for Ethiopian wolves and African wild dogs to protect these species.
On the other hand, traditional rabies control measures —such as indiscriminate wildlife culling— can conflict with conservation goals, damage populations, and destabilize ecosystems. Mass killing of bats or foxes is neither humane nor ecologically sound, and it may not be effective long-term. A more successful approach has been the use of oral vaccination for wildlife: in Europe and North America, vaccine-laden baits have been deployed to immunize foxes, raccoons, and other wild carnivores, significantly reducing —and in some areas, eliminating— rabies without mass culling.
In Latin America, specific strategies are being developed for vampire bats —for example, applying a topical gel containing vaccine or anticoagulant onto captured bats, which then spread it within colonies through self-grooming and social grooming. These innovative approaches aim to control the virus at its natural source, thereby protecting both animals and humans.
Another critical strategy is the One Health approach, which recognizes the interconnection between human, animal, and environmental health. Rabies provides a clear example: it requires collaboration among veterinarians, medical professionals, wildlife biologists, ecologists, and local communities. A One Health program may integrate:
Mass dog vaccination to protect humans
Livestock vaccination and improved enclosures to protect against bat attacks
Ecological studies on bat behavior
Public awareness campaigns on bite prevention
International health organizations actively promote this framework to eliminate rabies by 2030, acknowledging that no single sector can solve the problem alone. By monitoring rabies in wildlife, vaccinating at-risk animals (pets and livestock), and ensuring that exposed individuals receive timely PEP, we can minimize risks without compromising biodiversity.
Finally, public education plays a key role in reducing fear-driven indiscriminate killing. For example, teaching communities that bats are vital to ecosystems —they pollinate plants and control insect populations— helps encourage balanced management strategies. Rabies risk can be managed effectively without destroying colonies.
In conclusion, wildlife-associated rabies is a constant challenge, but one that is manageable through research, innovative vaccination methods, and cross-sector cooperation.
Conclusion for People Who Work with Animals
Rabies is one of the oldest and most deadly diseases known to humanity, but it is also 100% preventable with modern medicine. For those of us who work with or interact with domestic animals, wildlife, or livestock, the risk of exposure is higher, and prevention must be an absolute priority.
Pre-exposure vaccination (PrEP) is highly recommended for veterinarians, livestock farmers, researchers, wildlife caretakers, and field personnel, as it allows for a faster and more effective response in case of exposure. Additionally, knowing and correctly applying post-exposure prophylaxis (PEP) protocols is essential: washing the wound immediately, seeking medical attention, and receiving the vaccine can mean the difference between life and death.
People who work in close contact with bats, foxes, wild felines, jaguarundis, raccoons, monkeys, or stray dogs must be especially vigilant, as many of these species act as natural reservoirs of the virus.
It is important to remember that rabies is nearly 100% fatal once symptoms appear, but it is also nearly 100% preventable if action is taken promptly. Every vaccination campaign, every immunized animal, and every properly treated wound are steps toward a future free of rabies-related deaths.
Protecting yourself also means protecting your communities and ecosystems. Under the One Health approach, human, animal, and environmental health are interconnected. Prevention is not only a personal responsibility but also a collective commitment to conservation, science, and life.
References
Tarantola, A. et al. (2017). Four Thousand Years of Concepts Relating to Rabies in Animals and Humans. Tropical Medicine and Infectious Disease, 2(5): 5. (History of rabies) — clinmedjournals.org
Stanford Environmental Health & Safety — Rabies Virus Fact Sheet (Classification and structure of the virus) — ehs.stanford.edu
Bernal León, E. et al. (2021). Rabies in Costa Rica – Controlling Bat-Borne Rabies after Dog Rabies Elimination. Yale Journal of Biology and Medicine, 94(2): 311–329. (Rabies situation in Costa Rica) — pubmed.ncbi.nlm.nih.gov
World Health Organization (WHO) — Rabies: Key Facts (June 2024). (Global statistics, transmission, fatality, prevention) — who.int
Pan American Health Organization (PAHO) — Rabies in the Americas (Press release, September 21, 2018). (Achievements and data in Latin America) — paho.org
Rushford Health Library — Rabies (2024). (Symptoms in animals and humans, plain language resource) — rushford.org
BMC Veterinary Research (2019). Rabies Outbreaks in Cattle in Costa Rica. (Data on rabies transmitted by bats to livestock) — bmcvetres.biomedcentral.com
CDC — Badilla, X. et al. (2003). Human Rabies: A Reemerging Disease in Costa Rica? Emerging Infectious Diseases, 9(6): 721–723. (2001 rabies cases in Costa Rica) — stacks.cdc.gov
World Health Organization (WHO) — Zero by 30: Global Strategic Plan for Rabies (2018). (Elimination goal) — clinmedjournals.org
Additional References:
WHO Expert Consultation Reports on Rabies
CDC — Rabies Clinical Overview — who.int
Soares et al. (2024). Rabies in Jaguarundi (epidemiological source on wildlife rabies) — agris.fao.org
Comments